Ultrasound and vacuum studies elucidate the biomechanics of the infant suck cycle in breastfeeding
Intra-oral depth
Ultrasound imaging demonstrates that when the infant’s tongue is up during breastfeeding, the mid-tongue rests against the hard palate, the junction of the hard and soft palate, and the soft palate, sealing the oral cavity from the pharynx. An oral cavity seal is also required at the breast-face interface to generate baseline vacuum.
-
When the tongue is up, the intra-oral depth (IOD) is measured between the junction of the hard and soft palate (HSPJ) and the highest part of the tongue. The IOD when the tongue is up is often but not always 0 mm in successfully breastfeeding pairs.
-
That is, the apposition of the tongue and palate which comprises the pharyngeal seal mostly occurs between the mid-tongue and the junction of the hard and soft palate, but in 10% of cases may occur more posteriorly, between the soft palate and the most posterior part of the tongue, also known as the tongue base (which is not visible on oral examination).(1-3)
-
The base of the tongue has no anatomic connection with the lingual frenulum.(4)
Distance between the junction of the hard and soft palate and the nipple tip
The distance between junction of the hard and soft palate and the nipple tip is referred to by the acronym NHSPJD. When reflex depression of the mandible commences, the anterior and mid-tongue depress as a single unit, moving en bloc and in tandem with the mandible. The soft palate tracks the base of the tongue, which also moves inferiorly with the mid-tongue, both mid-tongue and base of the tongue tracking the mandible.
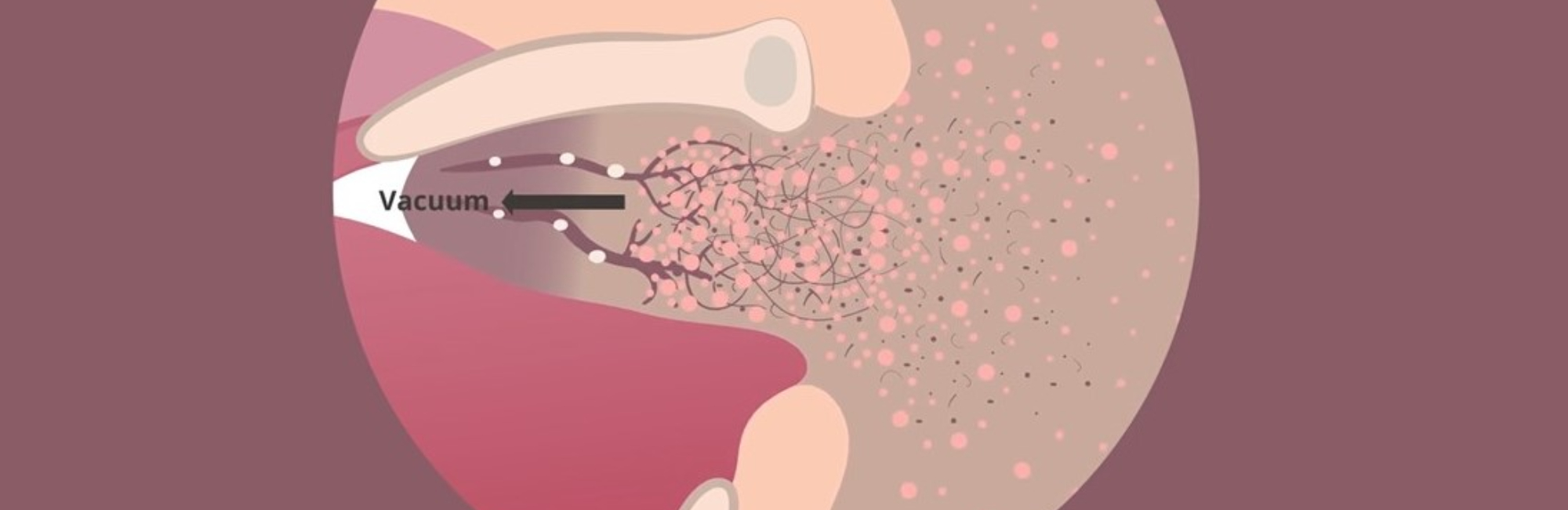
Intra-oral vacuums
Intra-oral vacuum (not tongue movement) drives milk transfer during breastfeeding, in tandem with contraction of the alveolar glands and dilation of the ducts during milk ejection. Peak vacuum is achieved when the mandible is extended, and is typically twice that of baseline vacuum.(5) The nipple ducts may become visible as milk fills the intra-oral space.
Intra-oral space
The intra-oral space is bordered distally by the nipple tip, proximally by the soft palate in apposition with the tongue base, superiorly by the hard palate, and inferiorly by the dorsal surface of the tongue, and does not contain air.(1-3, 6)
-
When the mandible is fully depressed and the tongue is down, the intra-oral depth (IOD) or depth axis continues to be measured as a line drawn between the junction of the hard and soft palate and the highest part of the tongue.
-
When the mandible is maximally depressed, the NHSPJD continues to be measured between the nipple tip and the depth axis.
-
The difference in NHSPJD between tongue up and tongue down indicates the degree of horizontal movement or slide of the intra-oral nipple and breast tissue during sucking.(1, 3)
Intra-oral nipple and breast tissue
In validation studies, nipple and breast tissue width dimensions (referred to in previous ultrasound studies as ‘nipple compression’ or ‘nipple diameter’) are measured at a distance of 2, 5, 10, and 15 mm proximal to the nipple tip in tongue up and tongue down.(1) The anterior portion of the tongue begins to rise slightly before the mid-tongue reaches its most inferior point. As the mid-tongue lifts to the palate with the rise of the mandible, milk passes between the soft palate and the tongue base.(1-3)
What ultrasound measures are linked with less maternal nipple pain and improved milk transfer?
The following ultrasound measures are associated with less maternal nipple pain and improved milk transfer:
-
Decreased distance between the nipple tip and junction of the hard and soft palate (NHPSPJ), both when the mandible is up and in full mandibular depression (‘improved’ nipple placement);
-
Expanded nipple and breast tissue dimensions;
-
Increased intra-oral dimensions (IOD, or ‘improved’ tongue shape);
-
Decreased nipple slide (distance the nipple tip moves between tongue up (TU) and tongue down (TD)).(1-3, 5, 7)
Recommended resources
The biomechanics detailed above are illustrated in animation (short) here and (long) here.
References
- McClellan H, Sakalidis VS, Hepworth AR, Hartmann PE, Geddes DB. Validation of nipple diameter and tongue movement measurements with B-mode ultrasound during breastfeeding. Ultrasound in Medicine and Biology. 2010;37:1797-807.
- Sakalidis VS, Williams TM, Garbin CP, Hepworth AR, Hartmann PE, Paech MJ, et al. Ultrasound imaging of infant sucking dynamics during the establishment of lactation. Journal of Human Lactation. 2013;29(2):205-13.
- Geddes DT, Sakalidis VS. Ultrasound imaging of breastfeeding - a window to the inside: methodology, normal appearances, and application. Journal of Human Lactation. 2016;32(2):340-9.
- Mills N, Keough N, Geddes DT, Pransky S. Defining the anatomy of the neonatal lingual frenulum. Clinical Anatomy. 2019;32:824-35.
- Geddes DT, Kent JC, Mitoulas LR, Hartmann PE. Tongue movement and intra-oral vacuum in breastfeeding infants. Early Human Development. 2008;84:471-7.
- Elad D, Povlovsky P, Blum O, Laine AF, Po MJ, Botzer E, et al. Biomechanics of milk extraction during breast-feeding. Proceedings of the National Academy of Science in the USA. 2014;111:5230-5.
- McClellan HL, Kent JC, Hepworth AR, Hartmann PE, Geddes DT. Persistent nipple pain in breastfeeding mothers associated with abnormal infant tongue movement. International Journal of Environmental Research and Public Health. 2015;12:10833-45. f.
